Aetna Health Insurance
For Addiction Recovery
OPEN 24/7 | PRIVATE ROOMS | SAME DAY ADMITS
Aetna, a prominent health insurance provider, has a rich history dating back to the early 20th century. During World War I, Aetna utilized its financial strength to provide insurance needed for government construction projects. In 1922, Aetna created the first insurer-owned rehabilitation clinic for disabled workers in Syracuse, NY. Over the years, Aetna has evolved to offer a wide range of insurance plans to meet the diverse needs of individuals and families.

Our Admissions Process
At Guardian Recovery, we are here to guide you every step of the way.
Our goal is to minimize stress during this potentially challenging time, making the transition into our program as smooth as possible.- Contact Us
Whether by phone, form, or text, we are standing by to help you find a treatment program that is right for you. - Personalized AssessmentWe ask the important questions, helping you develop an appropriate plan of action.
- AdmissionFrom travel plans to the day you arrive, we are standing by to assist you every step of the way.
"*" indicates required fields
Aetna Insurance Details
Insurance Overview
How Aetna Insurance Works
Aetna offers three main types of insurance plans: open-access plans, copay-only plans, and high-deductible plans. Open-access plans allow individuals to choose their doctors without needing a referral or a primary care physician. Copay-only plans ensure that costs after paying the deductible are limited to copays, with coverage for primary care physician visits and generic drugs before reaching the deductible. High-deductible plans offer preventative care services before meeting the deductible, sometimes coverage through a primary care physician with a copay, and the option of a health savings account.
Aetna also provides many local plans supported by a national network of providers to better support patients at the community level. Additionally, Aetna health insurance may qualify individuals for various alcohol treatment and drug addiction programs, such as detoxification, inpatient/residential rehabilitation, partial hospital treatment, intensive outpatient treatment, and continuing care programs (“alumni” programs). However, the specific coverage may vary, so it is important to check the plan or contact an Aetna representative to confirm the level of coverage, especially for out-of-network providers.
In summary, Aetna insurance offers a range of plans to cater to different needs, including substance abuse coverage, and provides avenues for members to appeal coverage determinations and seek external reviews when necessary. Understanding Aetna insurance and how it works is crucial for individuals and families to make informed decisions about their healthcare coverage. It is recommended to review the specific details of the insurance plan and consult with Aetna directly for more information.
Insurance Coverage
Aetna Insurance Coverage for Drug or Alcohol Rehab
Aetna drug rehab coverage depends on a member’s particular Aetna health plan and the addiction treatment provider they choose. There are many rehab centers that take Aetna insurance, including American Addiction Centers’ Recovery First Treatment Center in Hollywood, Florida; River Oaks Treatment Center outside of Tampa; Oxford Treatment Center in Etta, Mississippi; Greenhouse Treatment Center in the Dallas-Fort Worth area of Texas; and Desert Hope Treatment Center in Las Vegas. At AAC, we are in-network with Aetna health insurance and offer different levels of care for those with substance misuse issues and addiction. We are in-network with many insurance companies, including Aetna, which means that your addiction treatment could be covered fully or partially depending on your policy .
Aetna Coverage for Mental Health and Substance Abuse Treatment
Aetna provides coverage for mental health and substance abuse treatment. Members have access to a wide range of providers, including psychiatrists, psychologists, counselors, therapists, social workers, and primary care doctors. It is important to address mental health concerns if seeking care for substance misuse and addiction, as mental health problems can often co-occur with substance use.
To learn more about Aetna substance use and mental health coverage, members can access the online program provided by Aetna. This program allows members to view their coverage details, make claims, search for providers, and access other resources. Members can also visit the Find a Doctor portion of the Aetna website to search for providers.
Aetna Coverage for Outpatient Rehab
Aetna covers outpatient rehab services, which include a range of care levels based on the American Society of Addiction Medicine’s (ASAM) continuum of care. Basic outpatient services are level 1 within ASAM’s levels of care, which range from .5 to 4. However, level 2 (including 2.1 and 2.5) is also considered outpatient services, and these levels include intensive outpatient programs (IOPs) as well as partial hospitalization programs (PHPs).
With traditional outpatient rehab, patients stay in their own residences but attend individual and group treatment sessions at a healthcare, mental health, or treatment facility. Level 1 treatment typically involves fewer than 9 hours of services per week. With IOPs, services are similar to Level 1 outpatient services, but they’re on a more intense scale. Patients live at home and attend treatment during the day, in the evenings, or on the weekends at a treatment facility. PHPs, on the other hand, are often considered the midway point between inpatient and outpatient care. They provide slightly less-intense care than an inpatient rehab, but higher levels of care than a traditional outpatient program.
Thanks to the Affordable Care Act (ACA), all health insurance coverage (except grandfathered plans) must offer substance use disorder and mental health services. Plus, any plan purchased through the HealthCare.gov Marketplace can’t have a cap on the amount of substance use or mental health treatment covered.
Aetna Coverage for Therapy
Aetna and other insurance companies typically cover individual therapy, such as cognitive-behavioral therapy (CBT), for substance use disorders. The amount of coverage depends on a person’s specific health insurance plan and their chosen therapist.
In summary, Aetna insurance coverage for drug or alcohol rehab, mental health treatment, outpatient rehab, and therapy depends on the member’s specific Aetna health plan and the chosen provider. It is important to review the coverage details of the specific health plan and consult with Aetna or the provided contact number for more information
Insurance Plans
Aetna offers three main types of insurance plans: open-access plans, copay-only plans, and high-deductible plans. Open-access plans allow you to choose your doctors without needing a referral or a primary care physician. Copay-only plans guarantee that your costs after paying your deductible are limited to copays. Primary care physician visits and generic drugs are covered before you reach your deductible. High-deductible plans offer preventative care services before meeting the deductible, sometimes coverage through a primary care physician with a copay, and the option of a health savings account. You can log into the member website to view the details of your specific plan. Aetna also has many local plans that are supported by a national network of providers, providing better support at the community level. For example, American Addiction Centers frequently provides care for patients of Schaller Anderson Aetna Better Health networks in New York and Ohio. Please note that policy changes and errors can occur, so it is recommended to check with your insurance carrier directly to confirm coverage levels.Aetna Substance Abuse Coverage
If you have Aetna health insurance, you may qualify for several Aetna alcohol treatment and drug addiction programs, such as detoxification, inpatient/residential rehabilitation, partial hospital treatment, intensive outpatient treatment, and continuing care programs (“alumni” programs). However, the specific coverage may vary, so it is important to check your plan or contact an Aetna representative to confirm your level of coverage, especially for out-of-network providers. To learn more about your coverage with Aetna or find Aetna in-network inpatient rehab or outpatient substance abuse programs, you can call the number on your insurance card. For questions about drug or alcohol substance abuse coverage, it is recommended to contact your insurance provider directly for more information.Sources
- Types of Health Insurance Plans’ URL: https://www.aetna.com/health-guide/hmo-pos-ppo-hdhp-whats-the-difference.html
Organization Health Care Coverage’ URL: https://www.aetna.com/employers-organizations/health-plans/ppo-plans.html
Summary of benefits and coverage (SBC) | Aetna’ URL: https://www.aetna.com/individuals-families/member-rights-resources/summary-of-benefits.html
- Individual & Family Health Insurance Plans & Coverage | Aetna’ URL: https://www.aetna.com/individuals-families.html
Aetna State of Florida – HMO Plan’ URL: https://www.aetnastateflorida.com/hmo.html
My Health Insurance Plan Through Work | Aetna’ URL: https://www.aetna.com/individuals-families/member-rights-resources/health-insurance-through-work.html
Our history | Aetna’ URL: https://www.aetna.com/about-us/aetna-history.html
Health insurance plans | Aetna’ URL: https://www.aetna.com/health-care-professionals/patient-care/health-insurance-plans.html
Health insurance plans | Aetna’ URL: https://www.aetna.com/health-care-professionals/patient-care/health-insurance-plans.html
Guardian Recovery Locations
Our Facilities Transform Lives.
We believe that each level of care should serve as a catalyst for profound and lasting transformation. Our facilities are staffed by industry-leading professionals; pioneers in their respective fields. Through personalized care, we unlock the potential for lasting change, helping clients evolve and excel in all areas of their lives.
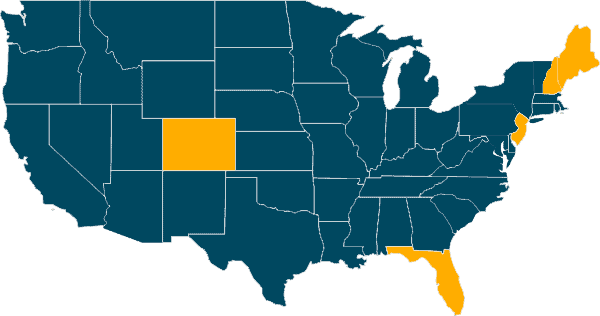

Delray Beach, Florida


Denver, Colorado

Largo, Florida

Pine Tree Recovery Center
Portland, Maine

Plymouth, New Hampshire

Pine Brook, New Jersey
Frequently Asked Questions
Yes, Aetna insurance provides coverage for drug and alcohol rehab. The specific coverage depends on the individual’s particular Aetna health plan and the chosen addiction treatment provider .
Aetna insurance policies have different options for inpatient and outpatient rehab, as well as other services to help on the path to recovery. This may include detoxification, inpatient/residential rehabilitation, partial hospital treatment, intensive outpatient treatment, and continuing care programs (“alumni” programs) .
To determine what your Aetna policy covers, you can call the phone number on the back of your insurance card or log in to your account on Aetna’s website. It’s important to check your policy benefits to determine which costs will be covered by Aetna and which will be out-of-pocket.
Yes, there are many rehab centers that accept Aetna insurance, including Guardian Recovery’ facilities located in various states across the U.S.
If Aetna denies coverage for addiction treatment based on medical necessity or regarding the experimental and investigational status, and the service or supply in question costs $500 or greater, the member may have an opportunity for an independent external review of the coverage denial. However, applicable state mandates take precedence for fully insured plans and self-funded non-ERISA plans.
Aetna offers resources and support for members struggling with drug or alcohol addiction. Members can reach out to Aetna for assistance in finding appropriate treatment options. Aetna Care Advocates, such as social workers, are available to provide guidance and support throughout the recovery process.
Coverage for out-of-network addiction treatment providers varies depending on the specific Aetna health plan. It’s important to check your plan or contact an Aetna representative to confirm the level of coverage for out-of-network providers.