Anthem Health Insurance
For Addiction Recovery
OPEN 24/7 | PRIVATE ROOMS | SAME DAY ADMITS
Anthem, Inc. is one of the largest health insurance companies in the United States, formed in 2004 through the merger of Anthem, Inc. and WellPoint Health Networks Inc., which has roots dating back to the 1940s. The company offers a wide range of health insurance products and services, including individual and family plans, employer-sponsored group health plans, and Medicare and Medicaid plans. Anthem is committed to improving the health and well-being of its members by providing access to quality, affordable healthcare.

Our Admissions Process
At Guardian Recovery, we are here to guide you every step of the way.
Our goal is to minimize stress during this potentially challenging time, making the transition into our program as smooth as possible.- Contact Us
Whether by phone, form, or text, we are standing by to help you find a treatment program that is right for you. - Personalized AssessmentWe ask the important questions, helping you develop an appropriate plan of action.
- AdmissionFrom travel plans to the day you arrive, we are standing by to assist you every step of the way.
"*" indicates required fields
Humana Insurance Details
Insurance Overview
Unlock the Power of Anthem Health Insurance for Your Addiction Recovery Journey
If you or a loved one is struggling with substance abuse, you may be wondering if your Anthem health insurance plan covers drug or alcohol rehab. The good news? Anthem is committed to helping members access the addiction treatment they need to reclaim their lives.
Anthem Covers Essential Health Benefits, Including Substance Abuse Treatment
Under the Affordable Care Act (ACA), all Anthem plans must cover essential health benefits – and that includes mental health and substance use disorder services. So whether you’re seeking inpatient rehab, outpatient care, or medication-assisted treatment (MAT), your Anthem plan likely provides at least partial coverage. The specific benefits depend on your plan details and location, but you can rest assured that Anthem is there to support your recovery journey.
Anthem’s Commitment to Behavioral Health and Addiction Recovery
Anthem understands that addiction is a complex disease that requires comprehensive, individualized care. That’s why they offer a robust network of behavioral health providers and resources to help members navigate the treatment process. From connecting you with in-network rehab centers to providing virtual therapy options through LiveHealth Online, Anthem is dedicated to making addiction treatment accessible and convenient. They even offer a 24/7 Behavioral Health Resource Center to help members find the right care for their needs.
Don’t Let Costs Stand in the Way of Your Recovery
Worried about the cost of rehab? Anthem’s plans often cover a significant portion of addiction treatment expenses, from detox to ongoing counseling and support. And with Anthem’s large network of providers, you’re more likely to find an affordable, in-network option that meets your needs.
With Anthem health insurance, you have the power to take control of your addiction and start building the healthy, fulfilling life you deserve. Don’t wait another day to begin your recovery journey. Reach out to an Anthem representative or an in-network rehab center today to verify your benefits and take the first step toward healing. Remember, you are not alone in this fight. Anthem is here to support you every step of the way – because your recovery is worth it.
Anthem Insurance: Your Partner in Addiction Recovery
Are you or a loved one struggling with addiction? You’re not alone. Millions of Americans face the challenges of substance abuse every day. But there’s hope. With the right treatment and support, recovery is possible. And if you have Anthem insurance, you may have access to comprehensive coverage for addiction treatment services.
Understanding Your Anthem Coverage
Anthem, part of the Blue Cross and Blue Shield (BCBS) network, offers a range of health insurance plans that include benefits for mental health and substance abuse treatment. Whether you have coverage through your employer, Medicaid, Medicare, or as a current or retired federal employee, Anthem has options to help you get the care you need. To get the most out of your Anthem coverage, it’s important to understand your specific plan. Contact Anthem directly by phone or log in to your member portal to learn more about your benefits, copays, and out-of-pocket costs. You can also reach out to addiction treatment facilities that work with Anthem, like Arista Recovery, for assistance in verifying your coverage.
Finding the Right Treatment Program
When it comes to addiction recovery, there’s no one-size-fits-all solution. That’s why Anthem covers a variety of treatment options, including:
- Inpatient rehab
- Partial hospitalization programs
- Outpatient services
- Medication-assisted treatment
The type of program that’s right for you will depend on factors like the severity of your addiction, your overall health, and your personal preferences. Working with an experienced addiction specialist can help you determine the best course of action. To maximize your Anthem benefits, look for in-network providers whenever possible. These facilities have negotiated rates with Anthem, which can help keep your out-of-pocket costs down. If you choose an out-of-network provider, you may still be able to work out a payment plan or use your out-of-network benefits.
Taking the First Step
Admitting you need help is never easy, but it’s the most important step on the road to recovery. With Anthem insurance on your side, you have the support you need to start your journey. Don’t wait another day to get the care you deserve. Reach out to a treatment provider or contact Anthem directly to learn more about your coverage and find a program that’s right for you.
Unlock the Power of Anthem Health Insurance for Your Addiction Recovery Journey
Are you or a loved one struggling with substance abuse? You’re not alone – and Anthem health insurance is here to support you every step of the way. With comprehensive coverage for addiction treatment, Anthem empowers you to get the help you need without breaking the bank.
Anthem’s Commitment to Substance Abuse Recovery
Anthem understands that addiction is a complex disease requiring personalized, evidence-based care. That’s why their plans cover a wide range of substance abuse services, including:
- Detox and withdrawal management
- Inpatient and residential rehab
- Outpatient programs and therapy
- Medication-assisted treatment (MAT)
No matter where you are in your recovery journey, Anthem has a plan to fit your needs and budget. From HMOs to PPOs to EPOs, you can choose the level of coverage that works for you – without sacrificing access to quality care.
Tailored Treatment Options for Lasting Recovery
With Anthem, you have the freedom to choose from a vast network of addiction treatment providers, ensuring you get the specialized care you deserve. Their plans cover:
- Dual diagnosis treatment for co-occurring mental health disorders
- Holistic therapies like yoga, art therapy, and mindfulness
- Telehealth services for convenient, discreet care
- Aftercare planning and relapse prevention support
Anthem’s integrated approach to addiction treatment addresses your unique needs, giving you the tools and support to build a strong foundation for lifelong recovery.
Navigating Your Anthem Addiction Coverage
Unsure about your specific benefits? Anthem makes it easy to understand your coverage and find the right provider:
- Log in to your member portal at anthem.com to view your plan details
- Use the “Find Care” tool to search for in-network addiction treatment providers
- Call the Member Services number on your Anthem ID card for personalized assistance
With Anthem by your side, you don’t have to face addiction alone. Their dedicated team is ready to guide you through every step of the insurance process, so you can focus on what matters most – your recovery.
Don’t let the cost of treatment stand in the way of your healing. Verify your Anthem coverage today and take the first step toward a brighter, addiction-free future. Your recovery is worth it – and Anthem is here to make it possible.
Sources
- https://www.anthem.com/individual-and-family/health-insurance-basics/essential-health-benefits/
- https://www.rehabs.com/insurance/anthem/
- https://www.anthem.com/coronavirus/blog/health-and-wellness/substance-use-recovery/
- https://www.anthem.com/individual-and-family/health-and-wellness/behavioral-health/
- https://www.anthem.com/provider/behavioral-health/
- https://www.anthem.com/coronavirus/blog/health-and-wellness/mental-health-support/
- https://www.anthem.com/individuals-families/member-resources/behavioral-health/
Guardian Recovery Locations
Our Facilities Transform Lives.
We believe that each level of care should serve as a catalyst for profound and lasting transformation. Our facilities are staffed by industry-leading professionals; pioneers in their respective fields. Through personalized care, we unlock the potential for lasting change, helping clients evolve and excel in all areas of their lives.
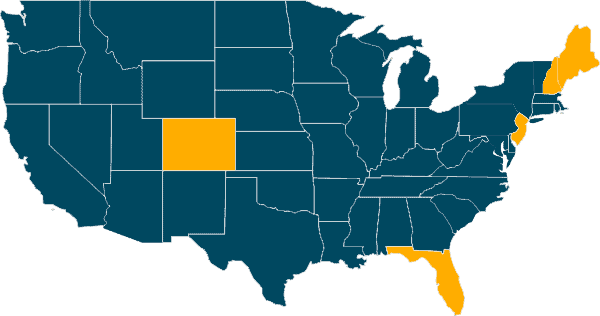

Delray Beach, Florida


Denver, Colorado

Largo, Florida

Pine Tree Recovery Center
Portland, Maine

Plymouth, New Hampshire

Pine Brook, New Jersey
Frequently Asked Questions
Yes, Anthem insurance plans typically offer coverage for substance abuse and mental health treatment, including addiction recovery services. The specific benefits and coverage levels will depend on your individual plan.
Anthem covers a range of treatment options for drug and alcohol addiction, such as:
- Detoxification
- Inpatient/residential rehab
- Partial hospitalization programs (PHP)
- Intensive outpatient programs (IOP)
- Outpatient services
- Medication-assisted treatment (MAT)
The appropriate level of care will be determined based on your specific needs and situation.
To verify your Anthem rehab coverage, you can:
- Call the member services number on the back of your insurance card
- Log in to your Anthem member portal online
- Contact the addiction treatment facility you’re considering and ask them to verify your benefits
Whenever possible, it’s best to select an addiction treatment center that is in-network with Anthem. In-network providers have negotiated rates with the insurance company, which can help lower your out-of-pocket costs. However, if you prefer an out-of-network facility, you may still be able to work out a payment plan with them.
The length of time your treatment will be covered depends on your specific Anthem plan and your individual treatment needs. It could range from 30 days to several months. Longer treatment durations are more likely to be approved for severe addictions. Your provider will work with Anthem to determine the appropriate length of treatment.
You may be responsible for some out-of-pocket expenses, such as:
- Deductibles
- Copays
- Coinsurance
The amount you’ll need to pay depends on your specific Anthem plan. Reviewing your benefits carefully and discussing costs with the rehab center can help you understand your financial responsibility.