A connection between substance use disorders (SUDs) and eating disorders is well-supported by research. Studies have shown that people who struggle with either eating disorders or SUDs are more likely to experience the other. One reason for this appears to be that both types of disorders often coexist with other mental health issues, which then tend to increase the risk of substance use and disordered eating to cope with symptoms. There are also certain risk factors that may increase the likelihood of developing both SUDs and eating disorders, such as a history of childhood neglect or abuse, low self-esteem, and emotional dysregulation.
Guardian Recovery offers integrated, individualized recovery programs that provide dual diagnosis treatment for substance use disorders and mental health conditions, seeking the most favorable outcomes for those we treat. Contact us today to learn more about your treatment options and our dedication to quality, effective care.
Recovery Starts
Here
Choose recovery and take control of your life, it’s the path to a brighter future filled with health, happiness, and fulfillment.
What Are Eating Disorders?
Eating disorders (EDs) are potentially severe mental health conditions that involve issues with eating behaviors, body weight, and self-image. These conditions can have significant physical and emotional repercussions and can be life-threatening if unaddressed. They can lead to serious complications such as malnutrition, electrolyte imbalances, heart problems, and even death.
Types of Eating Disorders Include:
- Anorexia Nervosa (AN)—This condition is characterized by a fear of gaining weight, a distorted body image, and a refusal to maintain a healthy body weight. People with AN typically drastically restrict their food intake, exercise excessively, and engage in other weight control-related behaviors such as purging or using laxatives.
- Bulimia Nervosa (BN)—This disorder is hallmarked by repeated episodes of binge eating followed by compensatory behaviors such as purging or excessive exercise. Individuals with BN may have a normal or slightly above-normal body weight.
- Binge Eating Disorder (BED)—This condition is characterized by recurrent episodes of binge eating, similar to those with bulimia, where the individual eats a large amount of food in a short period of time. However, individuals with this disorder do not engage in compensatory behaviors such as purging.
Other Specified Feeding or Eating Disorder (OSFED)—This category describes eating disorders that do not meet the diagnostic criteria of anorexia, bulimia, or binge eating disorder but still involve significant disruptions in eating behaviors.
Is There a Relationship Between Substance Use & Eating Disorders?
There are several reasons why substance use and eating disorders can be related. One possibility is that both behaviors can serve as coping mechanisms for dealing with underlying emotional distress. For example, a person may use drugs or alcohol to numb painful feelings, while another individual may use food as a way to deal with anxiety or depression.
Another possible explanation is that both disorders can be affected by environmental and social factors, such as peer pressure, media images, and cultural conventions. For example, individuals may feel pressured to use drugs or alcohol as a way to fit in with a certain group or control their weight to conform to unrealistic body standards.
That said, substance use and disordered eating can also have independent causes and risk factors. For example, genetics and family history may play a more significant role in the development of SUDs, while perfectionism and poor body image are more strongly associated with eating disorders.
What Is the Prevalence of Eating Disorders & Alcohol or Illicit Drug Use?
According to a 2020 study, SUDs, especially alcohol use disorders (AUDs), are commonly associated with eating disorders. (1) However, the prevalence of EDs and alcohol or illicit drug use varies depending on the population and the specific disorder being examined. For example, certain demographic groups, such as young adults and females, appear to be at higher risk for experiencing these conditions. The National Center on Addiction and Substance Abuse notes that approximately 50% of women with EDs have a SUD. (2)
A 2010 review found a high co-occurrence of EDs among women with SUDs. In one study examined, it was found that women with either a SUD or an ED were more than four times as likely to develop the other disorder as were women who had neither disorder. (3)
Complimentary Insurance Check
Find Out Today!
"*" indicates required fields
Risk Factors Associated With Substance Misuse & Eating Disorders
Several risk factors are associated with both substance misuse and eating disorders. Some of these risk factors are common to both disorders, while others are more specific to one or the other.
Common Risk Factors for SUDs & EDs Include:
- Genetics—The risk of experiencing a disorder may be higher if a family member also experiences it.
- Environmental Factors—Unresolved trauma, stress, and childhood abuse can contribute to the development of both disorders.
- Co-Occurring Mental Health Disorders—These include conditions such as depression, anxiety, and post-traumatic stress disorder (PTSD).
- Poor Self-Image—This includes having a negative body image, low self-worth, and poor self-esteem.
Specific risk factors for SUDs include peer pressure to use substances and the availability of drugs and alcohol. Those specifically for EDs include behaviors related to perfectionism, dieting, weight loss, and societal pressure to conform to body standards. Furthermore, having one or more risk factors does not necessarily mean an individual will develop a SUD or ED, but individuals who have one or more risk factors may be at increased risk.
Dual Diagnosis of Eating Disorders & Addiction (Co-Occurring Disorders)
A dual diagnosis refers to the presence of both a SUD and another mental health disorder, such as an ED. Dual diagnosis is common among individuals with SUDs, as substance use is often used as a way to self-medicate for underlying mental and emotional disturbances.
The co-occurrence of an ED and addiction can be particularly challenging to treat. Both disorders are associated with similar, potentially severe underlying factors, such as low self-esteem, impulsivity, and difficulty regulating emotions. Additionally, substance use can worsen eating disorder symptoms, and vice versa. Moreover, failure to effectively treat one condition may lead to a reemergence of the other.
Treatment Approaches for Substance Misuse & Eating Disorders
Integrated treatment approaches that address both disorders simultaneously are strongly advised for individuals with co-occurring SUDs and EDs. Treatment typically includes a combination of therapy, medication, and behavioral interventions.
Treatment Approaches & Strategies Include:
- Cognitive-Behavioral Therapy (CBT)—CBT aims to identify and alter negative thought patterns and behaviors that contribute to both disorders and help individuals establish healthy coping skills to manage triggers and prevent relapse.
- Dialectical Behavior Therapy (DBT)—DBT focuses on fostering mindfulness, emotion regulation, interpersonal effectiveness, and distress tolerance skills.
- Medication-Assisted Treatment (MAT)—MAT includes the use of medications to help manage withdrawal symptoms and cravings associated with drug or alcohol dependence. Medications may also be used to manage symptoms of co-occurring mental health conditions, such as depression and anxiety.
- Support Groups—12-step programs and other peer support groups can provide individuals with a sense of community and support as they work toward recovery.
- Family Therapy—This approach aims to address family dynamics that may contribute to SUDs and EDs and help family members acquire healthy communication patterns and improve coping strategies.
- Holistic Therapies—These activities include yoga, meditation, and acupuncture, which may be helpful in promoting relaxation and reducing stress.
Nutritional Rehabilitation
Nutritional rehabilitation is a key component of treatment for individuals with EDs. (4) This approach involves restoring and maintaining a healthy weight, as well as addressing any nutritional deficiencies that may have formed. It typically involves working with a registered dietitian or nutritionist who specializes in EDs, and the first step is to assess the individual’s current nutritional status, weight, body mass index (BMI), and any nutrient deficiencies.
Once the individual’s nutritional needs have been assessed, a treatment plan is constructed that involves a structured meal plan designed to provide them with the necessary nutrients to support their physical and emotional health and maintain a healthy weight. Nutritional rehabilitation may also involve nutrition education, counseling, and support. This can help individuals nurture a healthy relationship with food, learn about proper nutrition, and cultivate effective coping strategies to manage their triggers and prevent relapse.
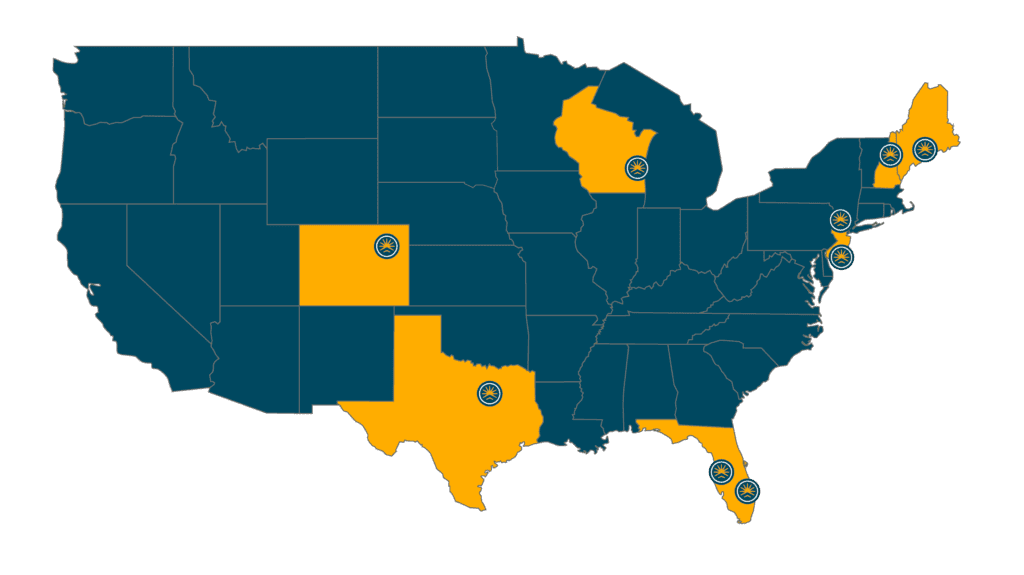
Our Locations
Our Facilities & Teams Transform Lives
Changing lives by providing comprehensive support and rehabilitation, empowering individuals to overcome addiction and regain control of their health and well-being.
Contact Guardian Recovery for Help With Co-Occurring Disorders Today
If you or a loved one are struggling with a substance use disorder, co-occurring eating disorder, or another medical or mental health condition, you are urged to reach out to Guardian Recovery for help. You can speak to an experienced, compassionate Treatment Advisor who can explain our streamlined admissions process and help you determine the level of care right for you. For a free, no-obligation health insurance benefits check, contact us today to begin your recovery journey.
SELF-ASSESSMENT:
Do I Have an Addiction Issue?
Disclaimer: Does not guarantee specific treatment outcomes, as individual results may vary. Our services are not a substitute for professional medical advice or diagnosis; please consult a qualified healthcare provider for such matters.