A recent study suggests that depression is a side effect of chronic opioid use, and adequate treatment of depression improves recovery outcomes.
According to the study published in The British Journal of Psychiatry, when patients adhered to a prescribed antidepressant and stopped using opioids, their depression symptoms subsided much more rapidly than patients who were also consistently taking an antidepressant, but continued to use opioids.
Start Healing Today!
Choose recovery and take control of your life, it’s the path to a brighter future filled with health, happiness, and fulfillment.
“We can’t be sure that a decrease in depression led to patients’ choosing to stop opioid use and we know prospective studies are needed,” said Jeffrey Scherrer, Ph.D., lead author and professor of family and community medicine at Saint Louis University. “Depression can worsen pain and is common in patients who remain long-term prescription opioid users. Our study should encourage clinicians to determine if their non-cancer pain patients are suffering from depression and aggressively treat patients’ depression to reduce opioid use.”
Researchers defined long-term opioid use for chronic, non-cancer pain as daily or near-daily use for at least 90 days. It’s estimated that between 1.4 and 10% of patients who receive a new opioid prescription will develop chronic opioid use, and 65 to 80% of patients who take opioids for 90 days are still taking them 3 to 5 years later.
Compared to short-term users, long-term users are significantly more likely to develop opioid use disorder or overdose. Long-term use is also associated with episodes of depression and treatment-resistant depression.
The study analyzed Veterans Health Administration medical record data collected from 2000 to 2012. A random 500,000-person sample was drawn from a possible 2,910,335 patients. Patients were ages 18 to 80 and without an HIV or cancer diagnosis. To qualify, patients must have had at least one outpatient visit in 1999 and 2000, and at least one annual visit between 2000 and 2001, during which they were not diagnosed with depression. All patients developed depression after more than 90 days of long-term prescription opioid use.
Complimentary Insurance Check
Find Out Today!
"*" indicates required fields
Researchers compared the likelihood of opioid cessation among patients who consistently used an antidepressant and those who did not. The antidepressants prescribed to patients in the study include selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), monoamine oxidase inhibitors (MAOIs), tricyclics (TCAs) and non-classified anti-depression medications.
“Effective depression treatment may break the mutually reinforcing opioid-depression relationship and increase the likelihood of successful opioid cessation,” Scherrer said.
Although this is not the first time prescription opioids have been linked with depression, this data better equips researchers to understand how they can develop adequate addiction recovery treatment that more effectively addresses the underlying causes and consequences of substance use. These findings demonstrate the importance of treating the co-occurring disorders that are either caused or exacerbated by substance use because we know that addiction does not occur on its own.
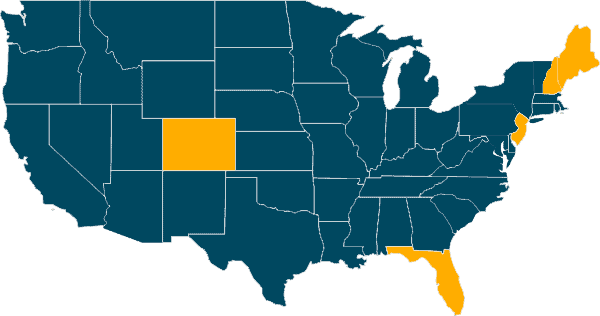
Our Locations
Our Facilities & Teams Transform Lives
Changing lives by providing comprehensive support and rehabilitation, empowering individuals to overcome addiction and regain control of their health and well-being.
Permanent recovery from opioid addiction is possible, and it starts with treatment that addresses physical and mental well-being. Contact a Guardian Recovery Specialist for more information about our Clinical Case Management program and our other services that can help you or someone you care about recover.
SELF-ASSESSMENT:
Do I have an Addiction issue?
Disclaimer: Does not guarantee specific treatment outcomes, as individual results may vary. Our services are not a substitute for professional medical advice or diagnosis; please consult a qualified healthcare provider for such matters.
Sources