Easier Access To Suboxone Saves Lives But At A Price
October 2022 marked the 20th anniversary of the U.S. Food and Drug Administration’s approval of Suboxone and Subutex, two prescription drugs that use the opiate-based medication buprenorphine to help treat opioid use disorders.
During those same two decades drug overdose rose to become the leading cause of accidental death in the U.S, with 60% of those deaths directly tied to an opiate.
Yet for much of that period, despite the growing awareness of the surging public health crisis, access to potentially life-saving medications containing
buprenorphine was limited at best and nearly impossible at worst. One recent study found that nearly 90% of Americans with an opioid use disorder are not receiving medically assisted treatments such as Suboxone.
In many parts of the country, especially rural areas, access to Suboxone was restricted by government regulations passed in response to the widely-held belief that easy access to large quantities of highly addictive painkillers such as Oxycontin contributed significantly to the rapid escalation in abuse of those medications.
The good news is that the federal government in recent years has taken measures to improve access to buprenorphine-based medications. The bad news is that improved access to Suboxone and Subutex has led to an increase in physical and mental dependence on the very medications prescribed to treat opioid addiction. I’ve seen this firsthand as a counselor in a treatment
facility.
Start Healing Today!
Choose recovery and take control of your life, it’s the path to a brighter future filled with health, happiness, and fulfillment.
Buprenorphine At Heart of Harm Reduction Movement
Buprenorphine is itself an opiate. Consequently, regular use – even when taken in compliance with a legitimately obtained prescription – can lead to addiction and withdrawal symptoms as severe as those of illicitly obtained heroin and Fentanyl.
Suboxone, the most widely prescribed medication for treating opioid use disorder, works by combining a small dosage of buprenorphine with naloxone, an opioid antagonist. The combination of the two medications works by blocking the receptors in the brain that not only cause cravings but also withdrawal symptoms such as nausea, aches and chills.
Suboxone and Subutex – as well as other medically assisted addiction treatments, such as Vivitrol, which is used for reducing alcohol and opiate cravings, and Narcan, which reverses the effects of opioid overdose – are at the center of the growing but still controversial harm reduction movement.
Harm reduction covers an array of treatment methods that don’t require complete abstinence from mind-altering substances. Instead, harm reduction methods are aimed at reducing the negative impact of drug use.
With that goal in mind, using an opiate-based medication such as buprenorphine to help reduce instances of fatal overdoses is viewed by harm reductionists as an overall positive, both for those who use drugs and society as whole.
Still, the idea of treating addiction with medications that contain opiates and can therefore be abused and possibly lead to addiction has long been shunned by abstinence-based treatment programs and remains controversial.
One study in Maryland, however, showed, that using these medications can reduce the risk of fatal overdoses by as much as 80%.
Suboxone is now widely used in detoxes to help opiate users through the difficult early days of withdrawal. The medication is generally prescribed in a taper protocol – eight milligrams on the first day, six milligrams on the second, four on the third, and so on down to nothing.
Suboxone Is Often Used After Detox To Ward Off Cravings
In the detox setting, Suboxone has proven invaluable in helping to keep clients suffering from the worst withdrawal symptoms – deep body aches and spasms, painful stomach cramps and nausea, chills and drenching sweats, profound feelings of anxiety and depression – from leaving treatment early against medical advice.
Many opiate users choose to continue using Suboxone after they complete detox to help ward off cravings in the weeks and even months after illicit opiate use is stopped.
Suboxone has proven especially useful in preventing overdoses in opiate users who relapse shortly after leaving treatment facilities, when the body is particularly vulnerable to the powerful effects of opioids.
But obtaining a prescription for Suboxone from a legitimate licensed medical professional can be difficult.
Indeed, in 2002 when Suboxone was approved for use to treat opiate addiction, only doctors who were board certified in addiction medicine or addictions psychiatry, or who had completed a certification course, were granted the necessary waiver to prescribe Suboxone. And each doctor was limited to prescribing to 30 patients.
The cap was initiated for a number of reasons. Not least was an effort to limit the overall amount of Suboxone being prescribed in a given area to prevent regions being flooded with the medication in the same way areas were overrun with Oxycontin.
The cap was raised to 100 patients in 2006 for physicians who’d already been prescribing the medication for more than a year.
Complimentary Insurance Check
Find Out Today!
"*" indicates required fields
Few U.S. Physicians Can Prescribe Suboxone
A 2021 study https://www.pewtrusts.org/en/research-and-analysis/reports/2021/09/buprenorphine-treatment-for-opioid-use-disorder-in-philadelphia found that just 6% percent of health care providers in Philadelphia were waivered to prescribe the medication. Moreover, studies have consistently shown that the number of physicians licensed to prescribe Suboxone was far greater in urban areas than rural regions.
Amid the COVID 19 epidemic, after it became clear people suffering from substance use disorders were being especially hard hit, the government eased some of those restrictions.
One significant shift was the ability of patients to obtain Suboxone prescriptions via telehealth – or a video conference – with a waivered physician. This was especially impactful in rural areas and for patients with handicaps that prevented them from physically visiting a doctor’s office.
Due to many accounts at the onset of the opioid crisis of doctors prescribing Oxycontin and other powerful pain medications without ever meeting with patients, the government had sought to curtail that by requiring an office visit.
But now many of the patients who benefitted from the easing of restrictions for obtaining Suboxone are discovering the downside to using an opiate-based medication to treat their substance use disorder.
Namely, that stopping usage of Suboxone, especially after a prolonged period of use, can be as difficult as stopping use of heroin or Fentanyl. Indeed, in some cases the withdrawal symptoms from buprenorphine can be so severe the user’s physician may recommend an inpatient, medically-assisted detox similar to those used for stopping use of heroin or Fentanyl.
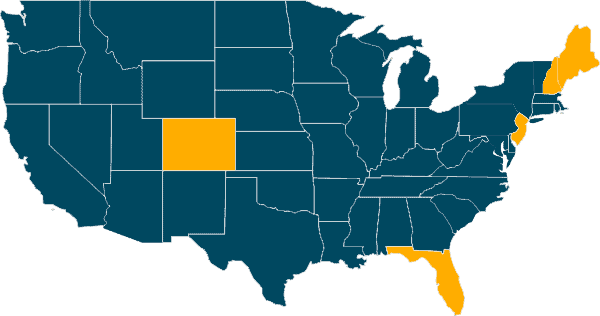
Our Locations
Our Facilities & Teams Transform Lives
Changing lives by providing comprehensive support and rehabilitation, empowering individuals to overcome addiction and regain control of their health and well-being.
Outpatient Programs Combine Medically Assisted Treatments and Tapering
In most cases, however, out-patient treatment is recommended, utilizing a
program tailored to the needs of the individual. These programs usually combine medically assisted treatments combined with a tapering protocol that gradually reduces the amount of buprenorphine taken. Non-addictive medications used during the tapering process include Clonidine, Buspirone and Vistaril, all of which ease withdrawal symptoms and reduce anxiety. The programs also involve intensive short-term monitoring and provide access to long-term counseling.
Naltrexone, an opioid blocker – or antagonist – similar to the naloxone found in Suboxone, is also increasingly being used as part of a comprehensive medically assisted treatment program for stopping use Suboxone.
Naltrexone has been widely prescribed for years in medications such as Vivitrol, which is used primarily as a long-term treatment for alcohol and opiate disorders. It works by blocking pleasure receptors in the brain triggered by use of alcohol and opiates.
SELF-ASSESSMENT:
Do I have an Addiction issue?
Disclaimer: Does not guarantee specific treatment outcomes, as individual results may vary. Our services are not a substitute for professional medical advice or diagnosis; please consult a qualified healthcare provider for such matters.
- https://www.sciencedirect.com/science/article/pii/S0955395922002031?via%3Dih
ub - https://nyulangone.org/news/medication-treatments-led-80-percent-lower-risk-fat
al-overdose-patients-opioid-use-disorder - https://www.pewtrusts.org/en/research-and-analysis/reports/2021/09/buprenorphi
ne-treatment-for-opioid-use-disorder-in-philadelphia