Mixing oxycodone and alcohol is extremely dangerous and can have serious health consequences. Both substances are central nervous system depressants, slowing down the body’s vital functions, such as breathing and heart rate. Combined, they can amplify these effects, leading to a potentially life-threatening situation.
Combining oxycodone and alcohol can also impair cognitive and motor function, leading to accidents, falls, and other injuries. Additionally, it can increase the risk of developing liver damage or other health problems.
If you are prescribed oxycodone, it is essential to follow your doctor’s instructions carefully and avoid drinking alcohol while taking the medication. Suppose you have a history of substance abuse or addiction. In that case, it is even more critical to prevent mixing oxycodone and alcohol, as it can increase the risk of overdose or other health problems.
If you or someone you know has mixed oxycodone and alcohol and is experiencing symptoms such as difficulty breathing, confusion, or loss of consciousness, seek medical attention immediately.
If you or someone you love has a substance use disorder, Guardian Recovery is available to help. We are dedicated to providing the most comprehensive and individualized medically monitored detox program. To learn more about our programs, contact us today.
Start Healing Today!
Choose recovery and take control of your life, it’s the path to a brighter future filled with health, happiness, and fulfillment.
Can You Mix Oxycodone With Alcohol?
No, it is not recommended to mix oxycodone with alcohol. Both oxycodone and alcohol are central nervous system (CNS) depressants, which slow down brain activity and can cause sedation, drowsiness, and respiratory depression. When taken together, the effects of both substances can be amplified, potentially leading to dangerous side effects such as decreased breathing, heart rate, blood pressure, and even coma or death.
Additionally, alcohol can increase the absorption of oxycodone in the bloodstream, leading to a higher risk of overdose. It is essential to follow the prescribing instructions for oxycodone and to avoid consuming alcohol or other CNS depressants while taking this medication.
What Is Oxycodone
Oxycodone is a strong prescription pain medication for treating moderate to severe pain. It belongs to a class of drugs called opioid analgesics, which work by binding to specific receptors in the brain and spinal cord to reduce pain signals.
Oxycodone is available in various forms, including immediate-release tablets, extended-release tablets, capsules, and liquid solutions. The immediate-release form is usually prescribed for acute pain, while the extended-release form is used for chronic pain that requires around-the-clock treatment.
While oxycodone can effectively manage pain, it also carries a risk of addiction, dependence, and overdose, mainly if misused or without medical supervision. Therefore, it is essential to use oxycodone precisely as a healthcare provider prescribes and follow all instructions and precautions carefully.
Understanding the Effects of Alcohol
Alcohol is a psychoactive substance that affects the brain and body in various ways. The effects of alcohol depend on several factors, including the amount consumed, the individual’s body weight, age, gender, and overall health.
Common Effects of Alcohol:
- Euphoria – Alcohol can produce euphoria and relaxation, which is why many people consume it recreationally.
- Impaired Judgment – Alcohol can impair judgment and coordination, making it difficult to perform tasks that require concentration and fine motor skills. This can lead to accidents, falls, and other injuries.
- Slurred Speech – Alcohol can affect speech, causing it to be slurred or difficult to understand.
- Memory Loss – Drinking too much alcohol can cause blackouts or gaps in memory.
- Dehydration – Alcohol is a diuretic that increases urine production and can lead to dehydration.
- Increased Heart Rate – Alcohol can increase heart rate and blood pressure, which can be dangerous for individuals with underlying heart or blood pressure problems.
- Digestive Problems – Alcohol can irritate the stomach lining and lead to digestive issues such as nausea, vomiting, and diarrhea.
- Addiction – Regular alcohol consumption can lead to addiction and dependence, causing withdrawal symptoms when alcohol use is stopped.
- Liver Damage – Long-term alcohol abuse can lead to liver damage, including cirrhosis, which is irreversible and life-threatening.
The Risks & Dangers of Mixing Oxycodone & Alcohol
The risks and dangers of mixing oxycodone and alcohol are significant and potentially life-threatening. Both oxycodone and alcohol are central nervous system (CNS) depressants, which can slow down brain activity and impair vital functions such as breathing, heart rate, and blood pressure.
Here are some of the specific risks and dangers of mixing oxycodone and alcohol:
- Respiratory depression.
- Increased risk of overdose.
- Impaired judgment and coordination.
- Liver damage.
- Increased risk of addiction.
Complimentary Insurance Check
Find Out Today!
"*" indicates required fields
What Happens if You Mix Painkillers With Alcohol?
Mixing painkillers with alcohol can be very dangerous and potentially life-threatening. Painkillers, also known as opioids or narcotics, are potent medications that relieve moderate to severe pain. Alcohol is a central nervous system depressant that can impair brain function and coordination.
When taken together, painkillers and alcohol can amplify each other’s effects and increase the risk of dangerous side effects such as drowsiness, respiratory depression, liver damage, and increased risk of overdose.
Side Effects
Mixing painkillers and alcohol can have various side effects, depending on the type and dosage of the painkillers and the amount of alcohol consumed.
Common Side Effects of Painkillers & Alcohol:
- Drowsiness and impaired motor function.
- Nausea and vomiting.
- Respiratory depression.
- Both painkillers and alcohol can cause liver damage, and taking them together can increase the risk of liver toxicity.
- Increased risk of overdose.
- Worsening of medical conditions.
- Impaired judgment.
Respiratory Depression
Respiratory depression is a severe side effect that can occur when alcohol and painkillers are taken together. Respiratory depression is the slowing down of breathing to a dangerous level, which can result in a lack of oxygen to the brain and other organs. This can be life-threatening and requires immediate medical attention.
Both painkillers and alcohol can depress the central nervous system, and when taken together, they can amplify each other’s effects. Opioid painkillers, in particular, can cause respiratory depression, especially when taken in high doses or combined with other medications that depress the central nervous system, such as alcohol.
Alcohol can also impair a person’s ability to recognize the signs of respiratory depression and seek help, which can further increase the risk of complications.
Sedation
Both painkillers and alcohol can cause sedation, which is a state of drowsiness or sleepiness. Together, they can amplify each other’s sedative effects, leading to increased drowsiness, impaired motor function, and slowed reaction times. This can be particularly dangerous when engaging in activities such as driving or operating heavy machinery.
Opioid painkillers, in particular, can cause significant sedation, and when combined with alcohol, the risk of sedation-related side effects increases. The sedative effects of painkillers and alcohol can also lead to falls, accidents, and other injuries.
Liver Damage
Both alcohol and painkillers can cause liver damage, and when taken together, the risk of liver toxicity increases. The liver is responsible for metabolizing both alcohol and painkillers, and when it is overloaded, it can become damaged.
Alcohol is a known hepatotoxin, which can damage liver cells and cause inflammation. The liver can become damaged from excessive alcohol consumption over time, leading to conditions such as alcoholic liver disease, cirrhosis, and liver failure.
Painkillers, particularly acetaminophen (found in medications such as Tylenol), can also cause liver damage when taken in high doses or over an extended period. The liver metabolizes acetaminophen, and when it is overwhelmed, it can cause liver cell damage, inflammation, and in severe cases, liver failure.
When alcohol and painkillers are taken together, the liver is forced to work harder to metabolize both substances, increasing the risk of liver damage.
Increased Risk of Overdose & Addiction
Taking alcohol and oxycodone together can increase the risk of overdose and addiction. Oxycodone is an opioid painkiller commonly used to treat moderate to severe pain. It works by binding to the opioid receptors in the brain and blocking pain signals.
When taken with alcohol, oxycodone can have an additive effect on the central nervous system, causing respiratory depression, sedation, and impaired motor function. This can lead to a higher risk of overdose, particularly when high doses of oxycodone or alcohol are consumed. Additionally, alcohol can increase the absorption of oxycodone, leading to higher levels of the drug in the bloodstream.
Combining alcohol and oxycodone can also increase the risk of addiction. Both substances can be habit-forming; using them together can lead to physical and psychological dependence. Over time, a person may require higher doses of oxycodone to achieve the same pain relief, leading to an increased risk of addiction and overdose.
How Long After Drinking Can You Take Painkillers?
It is generally recommended to wait at least a few hours after drinking alcohol before taking painkillers. The exact amount of time will depend on various factors, including the type of painkiller, the amount of alcohol consumed, and individual differences in metabolism.
Acetaminophen (found in medications such as Tylenol) and nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen and aspirin are commonly used for pain relief. Taking acetaminophen with alcohol can increase the risk of liver damage, so it is recommended to wait at least 2-3 hours after drinking before taking acetaminophen.
NSAIDs can also increase the risk of stomach bleeding and other gastrointestinal side effects when taken with alcohol, so it is generally recommended to avoid combining these medications with alcohol.
Is it Safe to Take Any Painkiller With Alcohol?
No, it is generally not safe to take any painkiller with alcohol. Combining painkillers with alcohol can increase the risk of side effects, including sedation, respiratory depression, liver damage, and overdose.
Additionally, alcohol can interact with other medications you may be taking, including prescription and over-the-counter medications.
Managing Pain Without Mixing Opioids With Alcohol
There are several ways to manage pain without mixing opioids with alcohol.
Alternative Pain Management Strategies:
- Non-opioid pain relievers.
- Physical therapy.
- Meditation, yoga, and relaxation exercises.
- Ice or heat therapy.
- Making lifestyle changes such as improving sleep, reducing stress, and exercising regularly.
- Acupuncture, chiropractic care, or massage therapy.
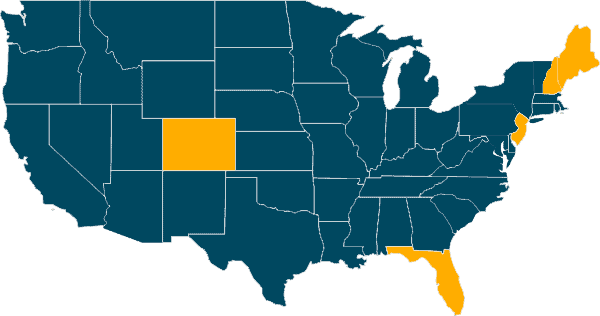
Our Locations
Our Facilities & Teams Transform Lives
Changing lives by providing comprehensive support and rehabilitation, empowering individuals to overcome addiction and regain control of their health and well-being.
Contact Us to Learn More
At Guardian Recovery, we remain dedicated to providing our clients with a comprehensive program of oxycodone detox that focuses on much more than physical stabilization. In addition to emphasizing physical recovery, we tackle mental, emotional, and spiritual well-being. While prioritizing a safe and pain-free cocaine withdrawal, we offer individual, group, and family therapy sessions, case management services, relapse prevention training, and aftercare planning.
Contact us today if you or your loved one is ready to begin an entirely new way of life and commit to long-term recovery. As soon as you call, we start developing a plan of action that begins with an initial pre-assessment. This assessment helps us determine the most appropriate level of care for each unique case. We identify potential coverage options if our medically monitored detox program is a good fit. We work closely with most major regional and national insurance providers. Contact us today for a free, no-obligation insurance benefit check.
SELF-ASSESSMENT:
Do I have an Addiction issue?
Disclaimer: Does not guarantee specific treatment outcomes, as individual results may vary. Our services are not a substitute for professional medical advice or diagnosis; please consult a qualified healthcare provider for such matters.
- https://www.drugs.com/food-interactions/oxycodone.html
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6761694/
- https://nida.nih.gov/publications/drugfacts/prescription-opioids
- https://www.mayoclinic.org/drugs-supplements/oxycodone-oral-route/proper-use/drg-20074193
- https://www.ncbi.nlm.nih.gov/books/NBK65500/
- https://www.niaaa.nih.gov/alcohols-effects-health/alcohols-effects-body
- https://nida.nih.gov/publications/drugfacts/prescription-cns-depressants
- https://uhs.umich.edu/combine
- https://www.nhs.uk/common-health-questions/medicines/can-i-drink-alcohol-if-i-am-taking-painkillers/
- https://www.fda.gov/media/99761/download
- https://pubs.niaaa.nih.gov/publications/arh25-2/101-109.htm
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5513682/
- https://www.cdc.gov/stopoverdose/polysubstance-use/index.html
- https://www.drugs.com/medical-answers/you-drink-alcohol-ibuprofen-3571982/
- https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/harmful-interactions-mixing-alcohol-with-medicines
- https://www.hhs.gov/sites/default/files/pmtf-final-report-2019-05-23.pdf